In the United States, nearly one in five adults—19.86%—are living with a mental illness, impacting over 49 million people. This staggering number reflects the widespread prevalence of mental health challenges across the nation. In addition to mental health concerns, 7.74% of the population, or more than 19 million people, are struggling with substance use disorder (SUD). The dual challenges of mental illness and substance abuse underscore the importance of accessible, comprehensive treatment options to support individuals in need.
In New York, the statistics closely mirror national trends, with 19.52% of the population, or approximately 2.97 million people, experiencing mental illness. Substance use disorder also affects a significant portion of New York residents, with 7.43%, or over 1.1 million individuals, grappling with addiction. These numbers highlight the critical need for targeted mental health and addiction services within the state, emphasizing the importance of localized support systems to meet the unique needs of its residents.
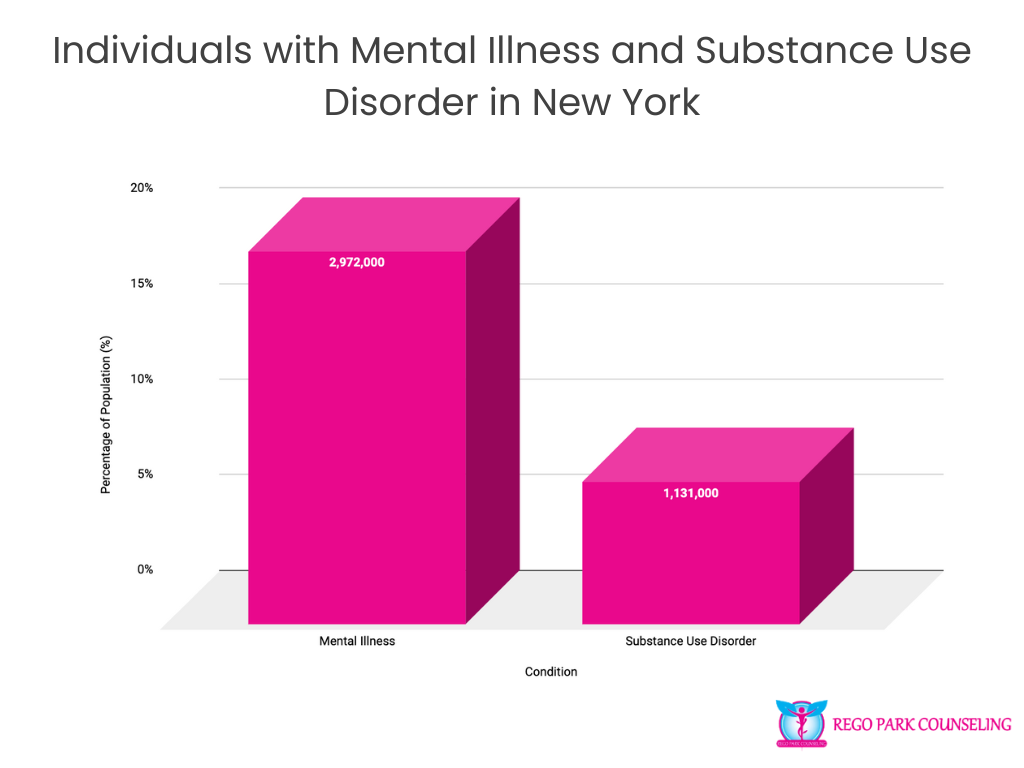
These statistics call for continued attention to mental health and substance abuse care, both on a national and state level, to ensure that the millions of individuals affected have access to the help they need.
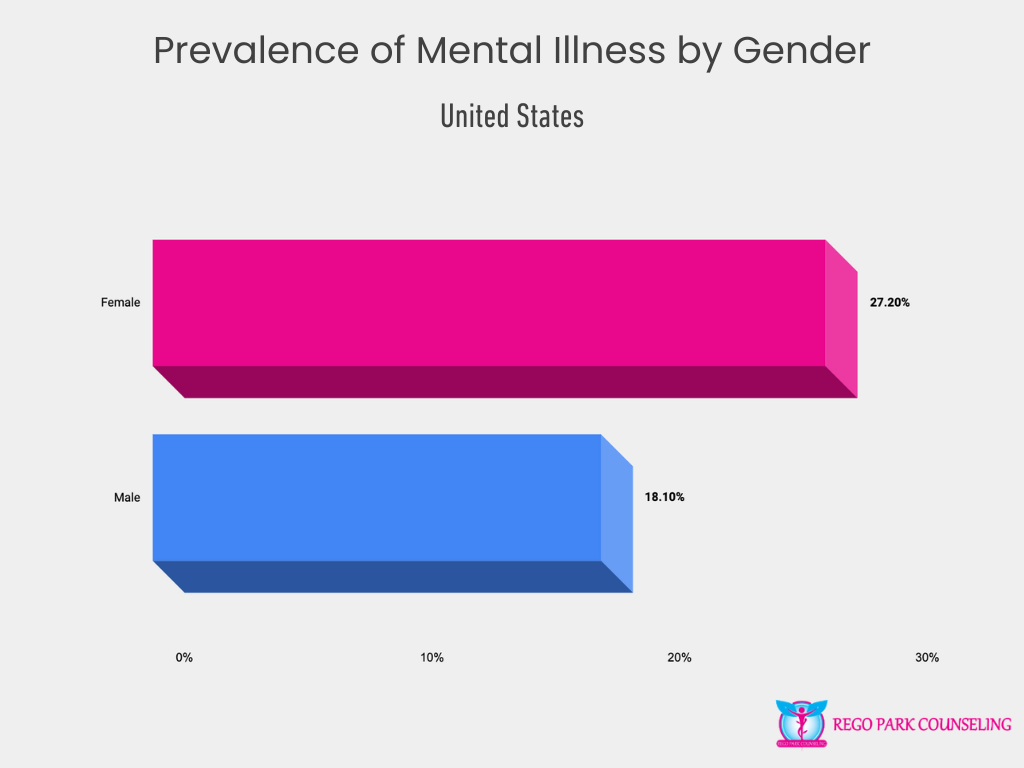
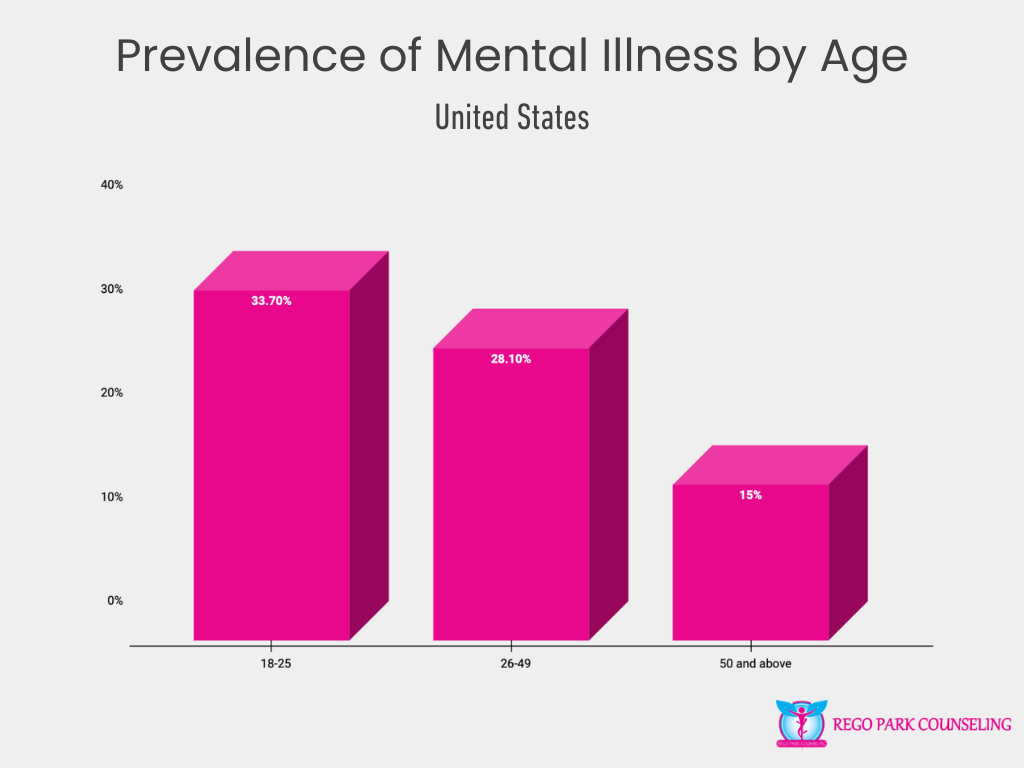
Mental illness affects individuals across all demographics in the United States, but the rates of prevalence vary significantly based on gender, age, and race/ethnicity. These variations highlight the complexity of mental health and the importance of understanding how different groups experience mental health challenges. By examining these demographic differences, we can better tailor mental health care and support to meet the specific needs of diverse populations, ensuring that treatment and resources are accessible and effective for everyone.
The prevalence of mental illness in the United States shows notable differences between genders. Women are disproportionately affected, with 27.2% experiencing mental health issues compared to 18.1% of men. This disparity may be influenced by various factors, including biological, social, and emotional differences, as well as gender-based societal pressures. Understanding the unique mental health needs of both genders is crucial in shaping appropriate interventions and support systems.
Young adults aged 18-25 face the highest rates of mental illness, with a concerning 33.7% reporting struggles with mental health. This figure decreases slightly for individuals aged 26-49, where 28.1% report mental health issues, and drops further to 15% for those aged 50 and above. The heightened prevalence among younger adults points to the need for targeted mental health resources and early intervention strategies to address challenges that often emerge during pivotal life transitions.
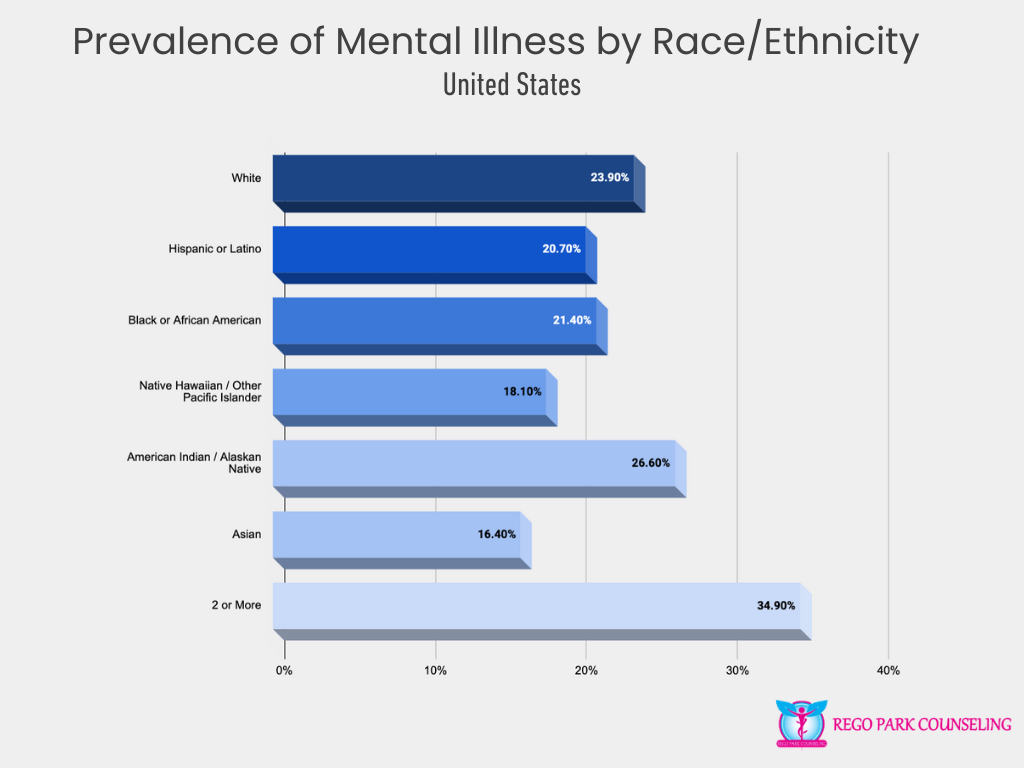
Mental illness affects various racial and ethnic groups at different rates, with the highest prevalence among individuals identifying as two or more races (34.9%) and American Indian/Alaskan Native (26.6%). White individuals also experience significant rates of mental illness (23.9%), followed by Black or African American (21.4%), Hispanic or Latino (20.7%), Native Hawaiian/Other Pacific Islander (18.1%), and Asian populations (16.4%). These statistics underscore the need for culturally sensitive mental health services that address the unique experiences and challenges faced by different racial and ethnic groups.
Tailored approaches to mental health care, informed by demographic factors such as gender, age, and race/ethnicity, are essential to meeting the diverse needs of individuals across the U.S.
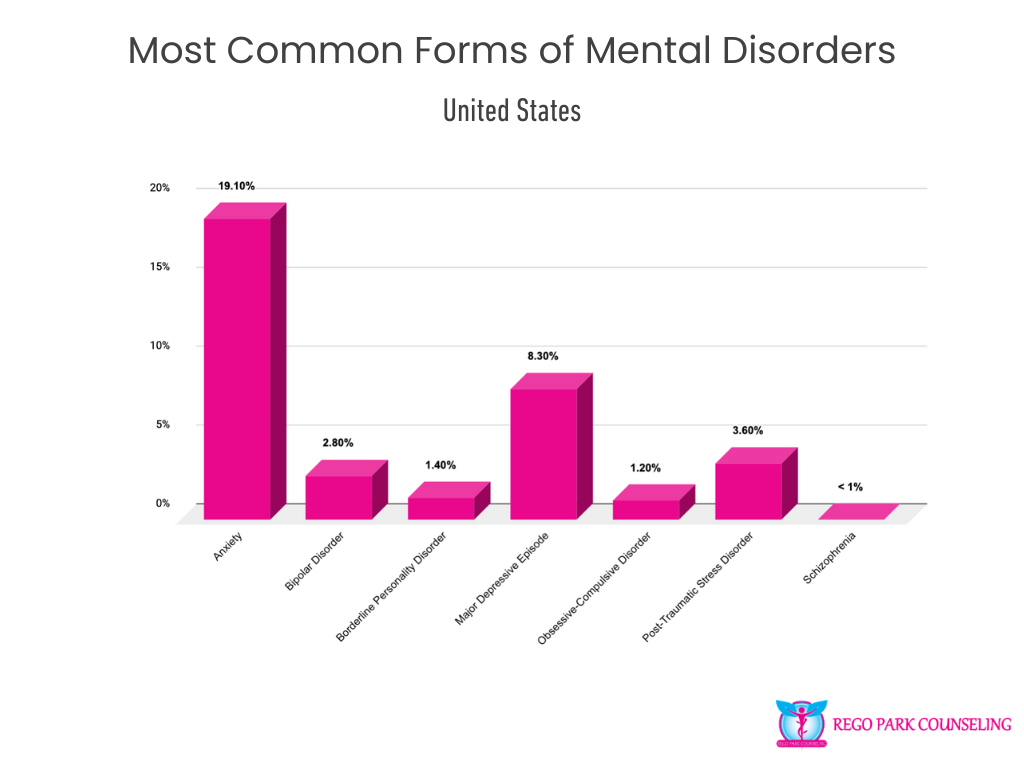
Mental health disorders manifest in various ways, affecting millions of people across the United States. Among the most common is anxiety, impacting 19.1% of the population. This condition often presents as excessive worry or fear and can significantly disrupt daily life. Major depressive episodes follow closely, with 8.3% of individuals experiencing severe periods of low mood and loss of interest, further underscoring the prevalence of mood-related disorders.
Other mental health conditions affect smaller percentages but remain critical to address. Post-traumatic stress disorder (PTSD) impacts 3.6% of the population, often triggered by traumatic experiences, while bipolar disorder, which involves extreme mood swings, affects 2.8%. Borderline personality disorder, obsessive-compulsive disorder (OCD), and schizophrenia, although less common, still affect millions of Americans, with OCD at 1.2%, borderline personality disorder at 1.4%, and schizophrenia affecting less than 1%.
Each of these disorders requires targeted care and intervention, highlighting the need for ongoing mental health support and treatment options across the country.
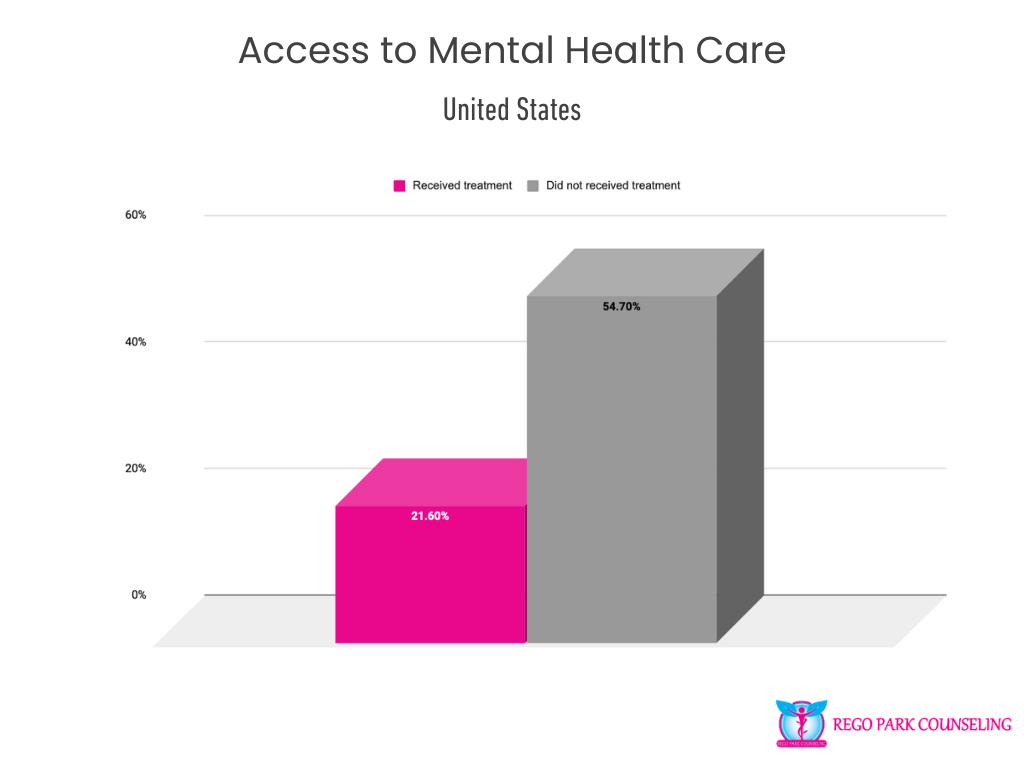
Access to mental health care remains a significant challenge in the United States. While 21.6% of adults have received some form of mental health treatment, more than half—54.7%—have not received the care they need. This gap in treatment access highlights the barriers many individuals face, whether due to stigma, cost, lack of insurance, or limited availability of services. Ensuring that more people can access the necessary mental health support is essential for improving overall mental well-being across the nation. Increased awareness, better coverage, and expanded services are critical steps in closing this treatment gap.
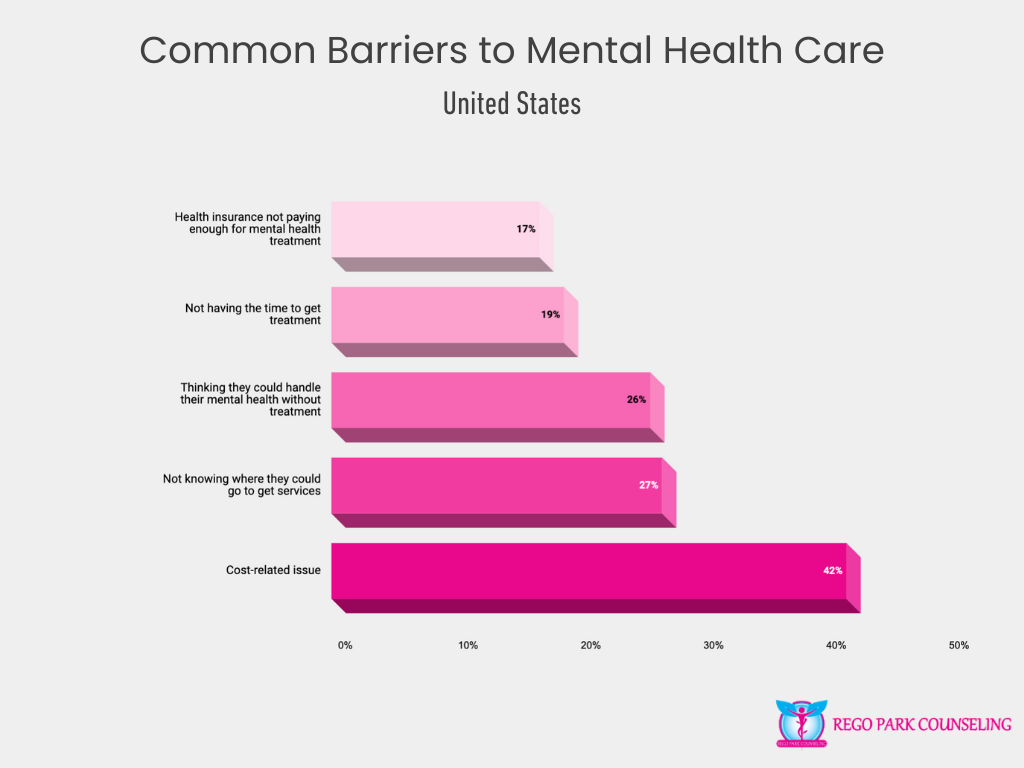
Many individuals in the U.S. face significant barriers when trying to access mental health care services. Cost is the most prominent issue, with 42% of individuals citing financial constraints as a major obstacle to receiving treatment. In addition, 27% of people report not knowing where to seek mental health services, underscoring the need for better mental health education and resource availability.
Some individuals (26%) believe they can manage their mental health issues without professional treatment, which may reflect societal stigma or a lack of understanding about the importance of mental health care. Time constraints also play a role, with 19% of people finding it difficult to carve out time for treatment, while 17% experience issues related to inadequate health insurance coverage for mental health services.
Addressing these barriers is crucial to ensuring more individuals can access the mental health care they need, whether by reducing costs, expanding insurance coverage, or increasing awareness about available services.
Among adults aged 18 or older in the U.S., 21.8% have received some form of mental health treatment, reflecting the ongoing demand for mental health services across the country. The most common form of treatment is the use of prescription medication, with 15.2% of adults relying on medication to manage their mental health conditions.
Outpatient services are also widely utilized, with 13.7% of adults receiving mental health care through outpatient programs. Of these, 10.7% access treatment in specialized facilities, rather than general medical clinics or doctors’ offices, emphasizing the importance of dedicated mental health services. Telehealth has grown significantly, with 12.1% of individuals engaging in virtual mental health care, providing a flexible and accessible option for many.
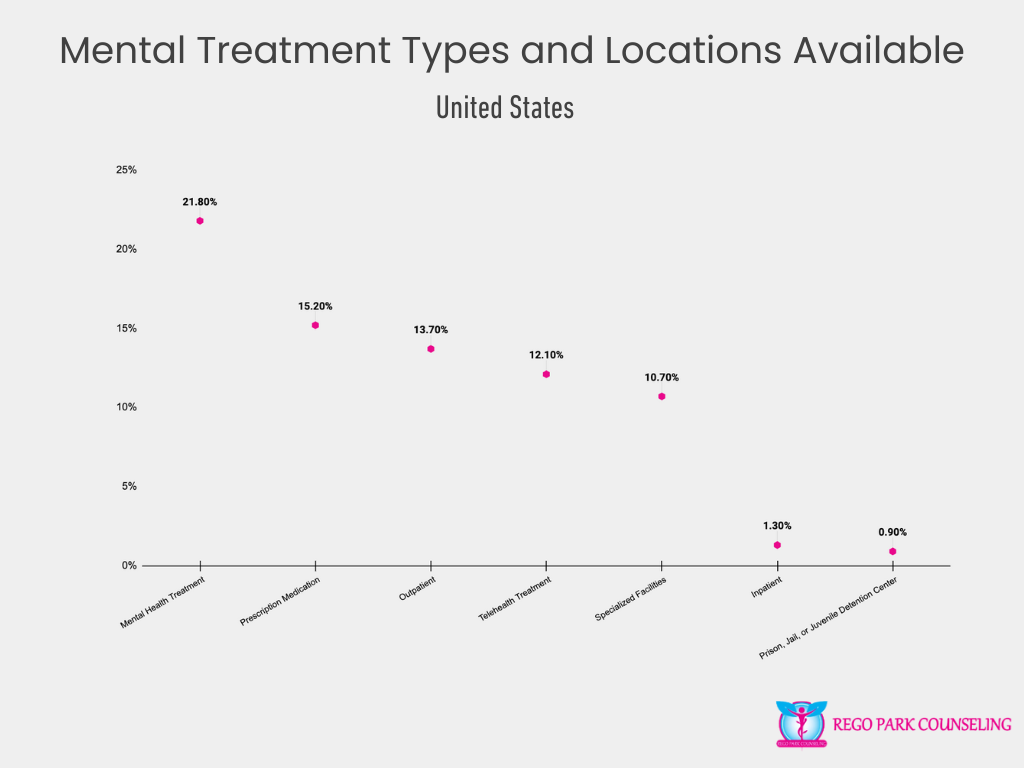
Inpatient treatment, which involves more intensive care in a residential setting, is less common but still critical for some, with 1.3% of adults receiving care in this manner. Additionally, 0.9% of individuals have received mental health treatment while in prison, jail, or juvenile detention centers, underscoring the need for mental health services across various institutional settings.
These statistics highlight the variety of treatment types and locations available, as well as the importance of continuing to expand access to care in order to meet the diverse needs of individuals seeking mental health support.
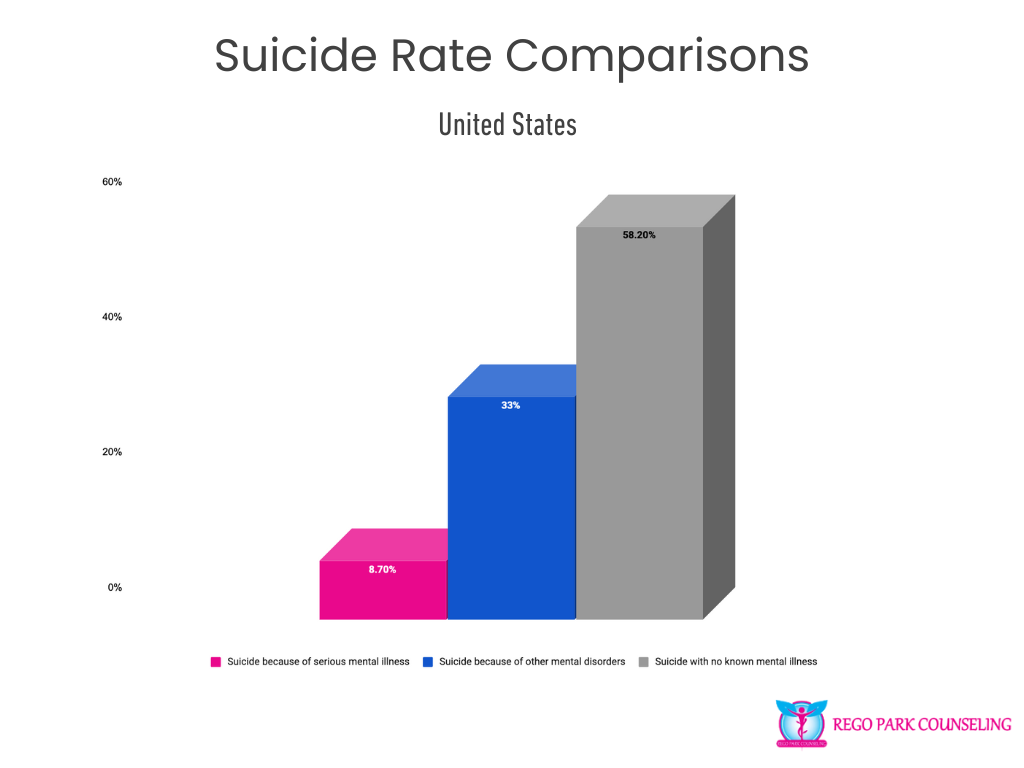
Suicide remains a complex issue in the U.S., with a range of underlying causes. Among those who die by suicide, 8.7% are attributed to serious mental illnesses, such as schizophrenia or bipolar disorder. A larger percentage—33%—are linked to other mental disorders like anxiety or depression. However, a staggering 58.2% of suicides occur among individuals with no known mental illness. These statistics underscore the critical need for early intervention, better mental health awareness, and broad-based support systems to prevent suicide, especially for those who may not present obvious signs of mental health struggles.
Substance use in the United States affects a wide range of individuals, but the prevalence and patterns of use vary across demographic groups. Factors such as age, gender, race/ethnicity, and employment status all influence the likelihood of substance use, reflecting the complex social, cultural, and economic forces at play. Understanding these differences is essential for creating effective prevention and treatment strategies that are tailored to the unique needs of each group. The following sections explore the rates of substance use across various demographics, shedding light on the populations most impacted by substance-related challenges.
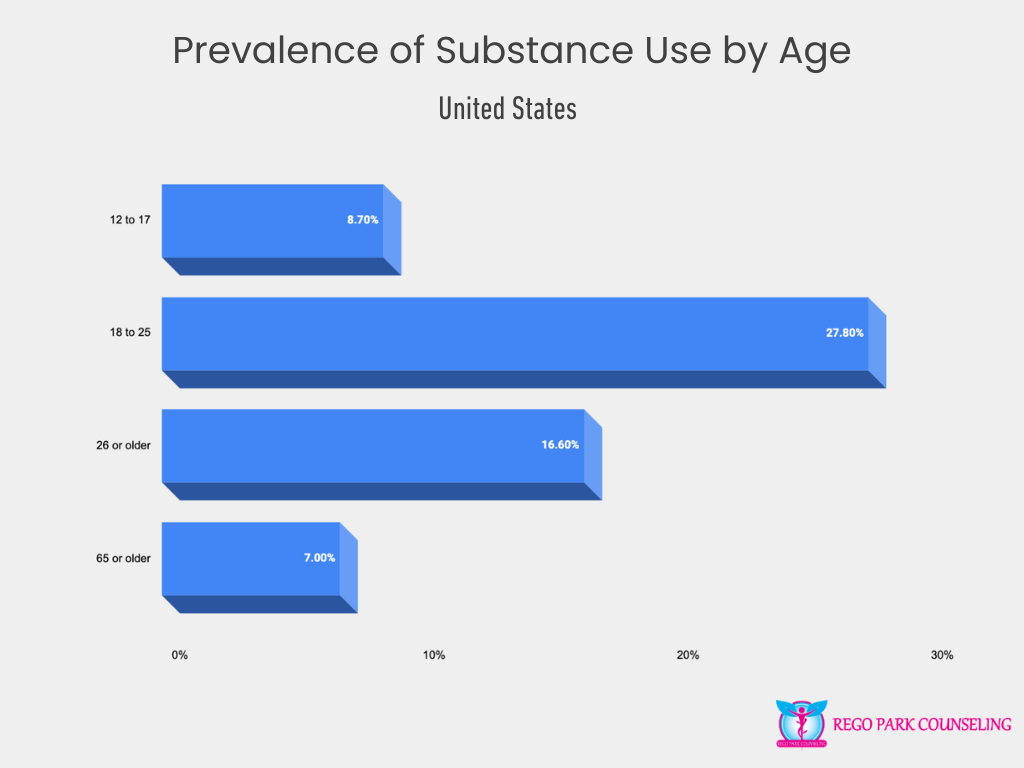
Substance use varies significantly by age group, with the highest rates occurring among young adults. Those aged 18 to 25 report the most substance use, with 27.8% engaging in substance-related activities. This age group is often exposed to increased social pressures and life transitions, contributing to higher rates of use. Among adolescents aged 12 to 17, 8.7% report substance use, a concerning statistic that calls for early intervention and prevention efforts. For adults 26 and older, substance use decreases to 16.6%, while the lowest rate is found among those 65 and older, at 7%. These figures demonstrate that substance use trends tend to peak in early adulthood and decline with age.
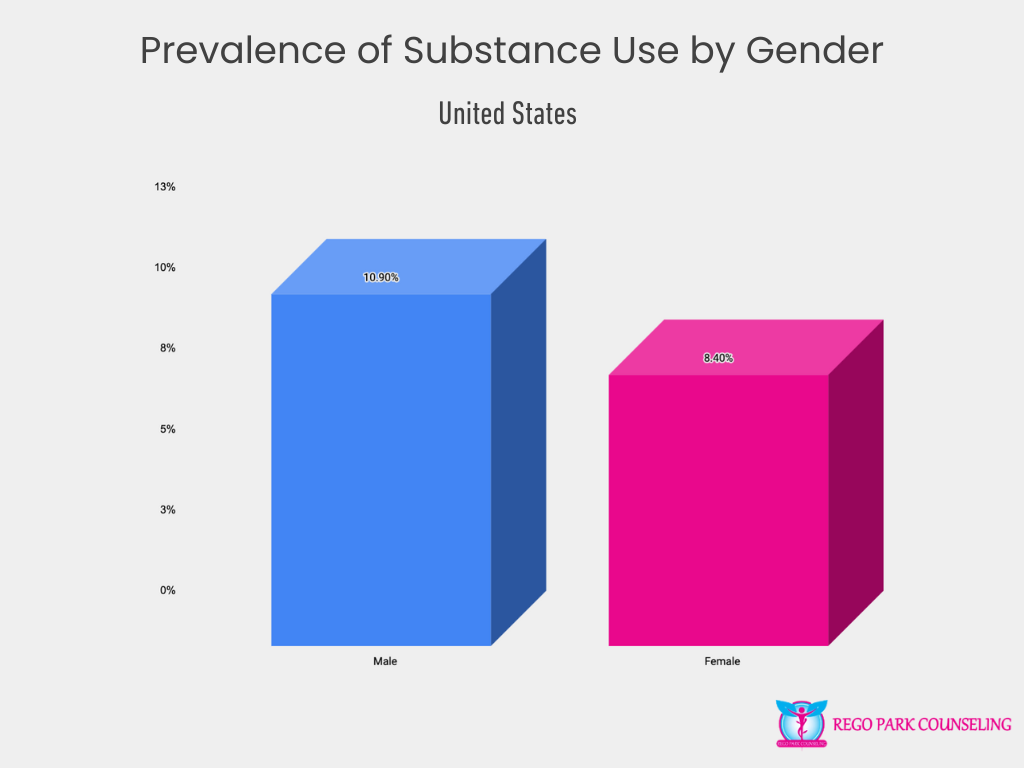
Gender also plays a role in substance use, with men more likely to report use than women. Specifically, 10.9% of males engage in substance use compared to 8.4% of females. This difference may stem from social, cultural, and biological factors that influence risk behaviors. Understanding these gender differences is essential for creating tailored substance use prevention and treatment programs.
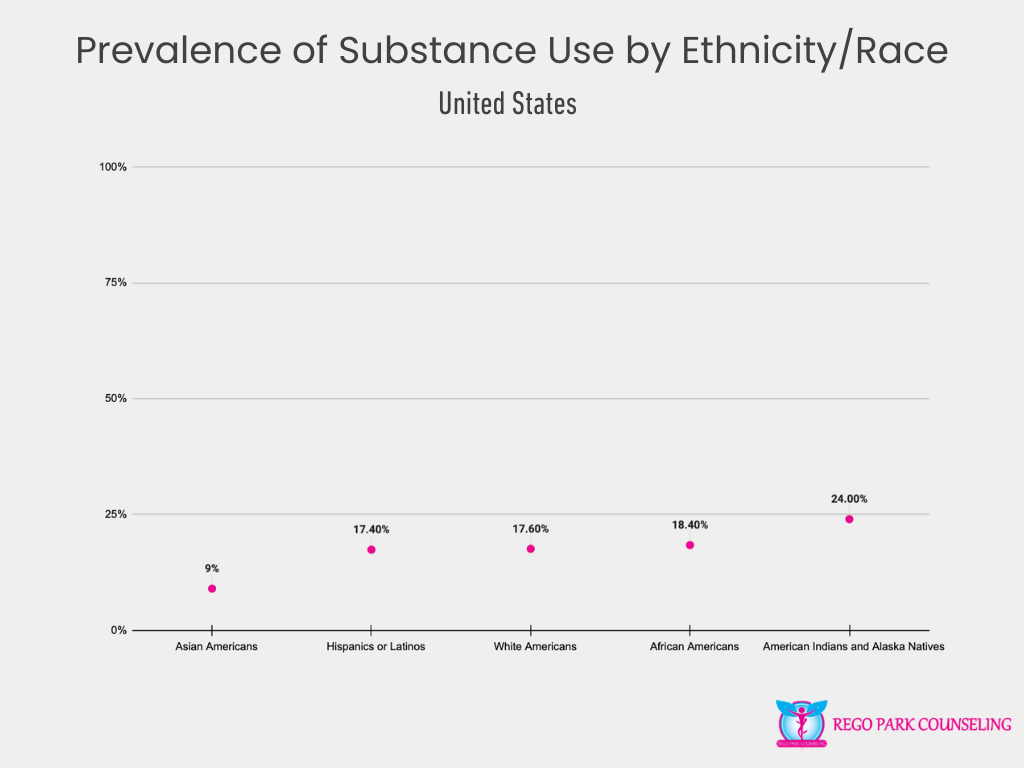
Substance use varies across different racial and ethnic groups in the U.S. American Indians and Alaska Natives have the highest reported substance use rate at 24%, reflecting a critical need for targeted support and culturally relevant interventions in these communities. African Americans report a substance use rate of 18.4%, followed by White Americans at 17.6%, and Hispanics or Latinos at 17.4%. Asian Americans report the lowest rate of substance use, at 9%. These differences suggest that cultural, economic, and social factors may influence substance use behaviors across these communities, highlighting the importance of culturally sensitive approaches to treatment and prevention.
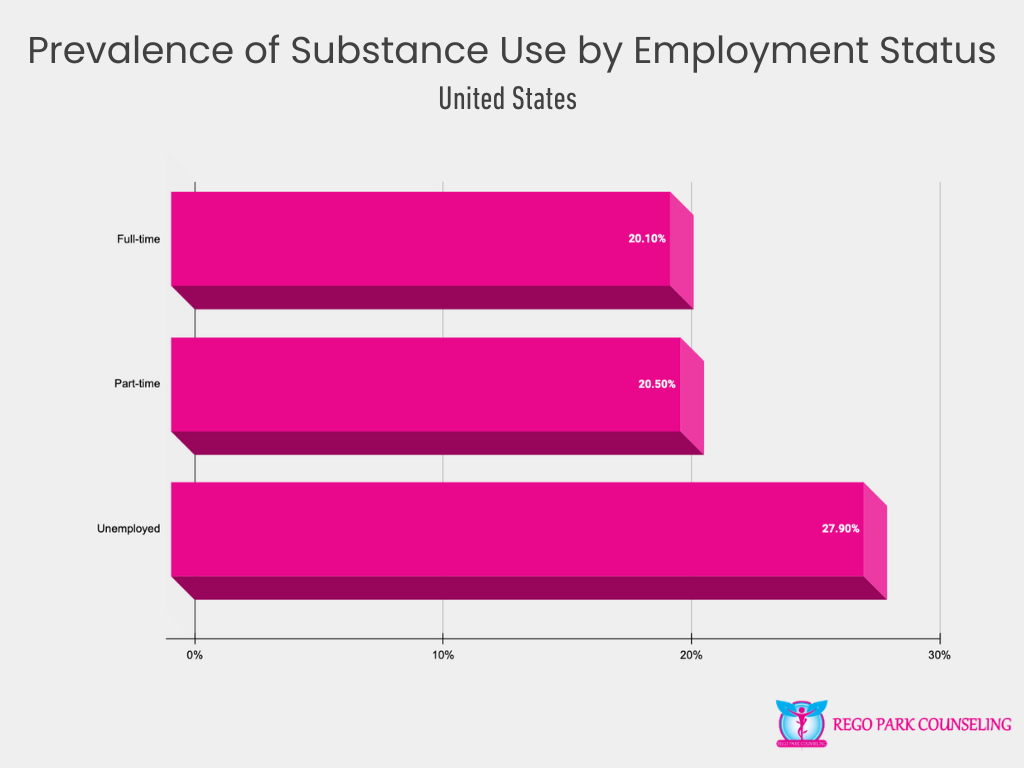
Employment status significantly impacts substance use rates, with unemployed individuals reporting the highest rate at 27.9%. This figure suggests a strong connection between economic insecurity and substance use, as those without jobs may experience heightened stress, lack of purpose, or social isolation, increasing their risk of substance use. Individuals working part-time report a slightly higher rate of substance use (20.5%) compared to those working full-time (20.1%). These statistics point to the importance of addressing mental health and substance use issues within the context of employment, offering resources and support to those struggling with addiction in both workplace and unemployment scenarios.
Addiction to specific substances in the United States presents a varied landscape, with alcohol leading as the most commonly abused substance. At 10.5%, alcohol addiction affects a significant portion of the population, often due to its widespread availability and social acceptance. Marijuana follows, with 6.7% of individuals reporting addiction, reflecting its increasing use and legalization in many states.
Opioid addiction, encompassing both prescription and illicit drugs, impacts 3.8% of the population and remains a critical public health issue due to its strong link to overdose deaths. Pain relievers also contribute significantly, with 2% of individuals reporting misuse. Tranquilizers, sedatives, and prescription stimulants each account for 0.8% of addictions, while heroin (0.3%) and cocaine (0.5%) are less common but remain dangerous and highly addictive substances.
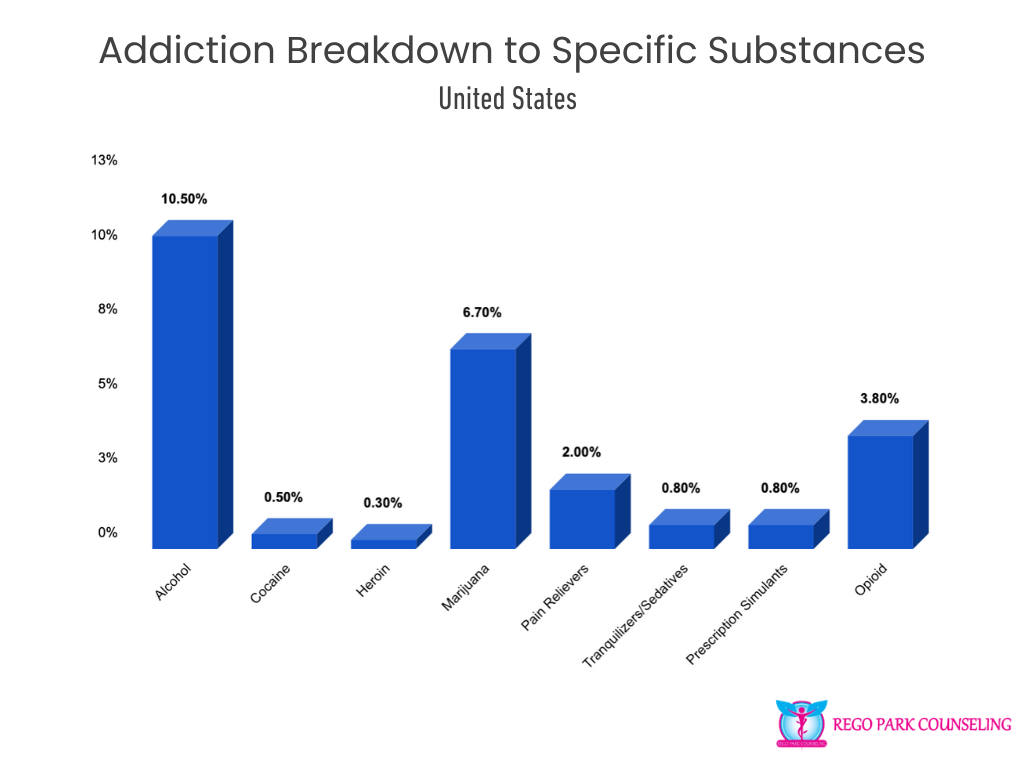
This breakdown highlights the diverse range of substances contributing to addiction across the U.S., emphasizing the need for specialized treatment programs that address each substance’s unique challenges and impacts.
Addressing substance abuse requires comprehensive treatment programs that cater to the diverse needs of individuals struggling with addiction. From counseling and behavioral therapies to medical interventions and support groups, substance abuse treatment aims to provide a pathway to recovery and long-term wellness. Despite the availability of various treatment options, access and utilization of these services remain a challenge for many. The following sections will explore key aspects of substance abuse treatment, highlighting the effectiveness, accessibility, and challenges surrounding the recovery process in the U.S.
Despite the availability of substance use treatment programs, many individuals do not seek the help they need. The most common reason—reported by 36.7% of individuals—is not being ready to stop using, underscoring the complexity of addiction and the challenge of recognizing when help is needed. Financial barriers also play a significant role, with 24.9% citing lack of healthcare coverage and high treatment costs as obstacles to receiving care.
Other barriers include not knowing where to go for treatment (17.9%) and not finding a program that offered the type of treatment they wanted (15.8%). Some individuals (15%) believe they can manage their addiction without professional help, which may be linked to stigma or misconceptions about treatment. Additionally, 14.7% of people worry that seeking treatment could negatively impact their job, highlighting the fear of social and professional consequences.
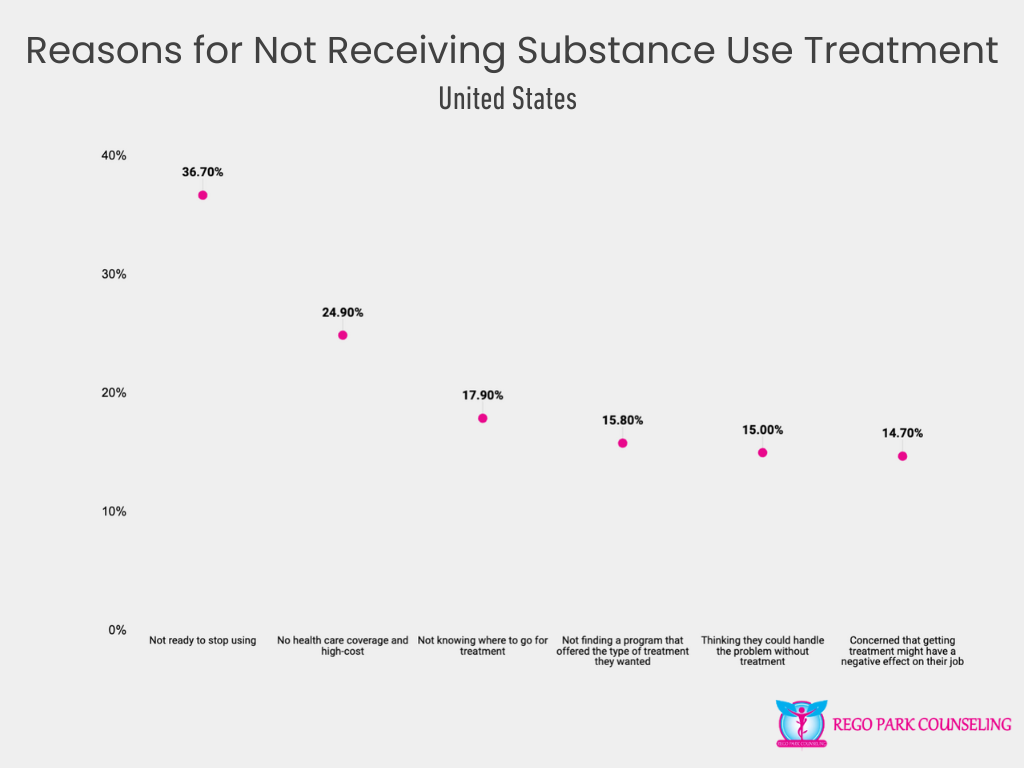
These statistics reveal the many barriers that prevent individuals from accessing the substance use treatment they need, emphasizing the importance of improving education, reducing stigma, and increasing access to affordable, flexible care.
Recovery from mental health and substance use issues is not only possible but a reality for many individuals. Among adults who have faced mental health challenges, 66.5% consider themselves to be in recovery or fully recovered, illustrating the impact that effective treatment and support can have on mental well-being. When it comes to recovery from drug or alcohol use problems, the success rate is even higher, with 72.2% of individuals reporting that they are in recovery or have overcome their addiction.

These recovery rates provide hope and reinforce the importance of accessible treatment options, long-term support, and community resources for individuals on their journey to wellness. The positive outcomes experienced by those in recovery highlight the potential for transformation, even after struggling with mental health or substance use disorders.
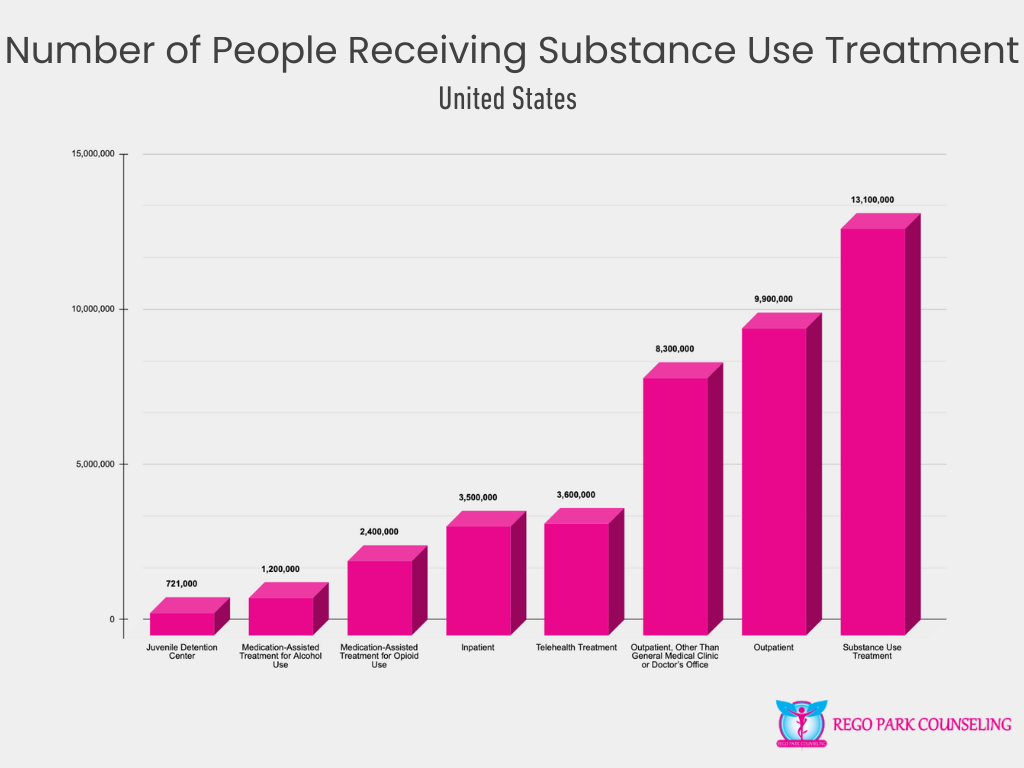
In the U.S., 13.1 million individuals are actively receiving substance use treatment, reflecting the widespread need for addiction services. The majority of those receiving treatment, around 9.9 million, are engaged in outpatient programs, which allow individuals to receive care while maintaining their daily routines. Of those, 8.3 million people are participating in outpatient services provided by specialized treatment centers rather than general medical clinics or doctors’ offices.
Telehealth has become an increasingly vital part of treatment, with 3.6 million people utilizing virtual platforms for their care. Inpatient treatment remains critical for individuals requiring more intensive care, with 3.5 million people receiving substance use services in residential facilities. For opioid addiction, medication-assisted treatment (MAT) plays a significant role, with 2.4 million individuals receiving MAT, while 1.2 million individuals are undergoing medication-assisted treatment for alcohol use disorders.
Additionally, 721,000 individuals in juvenile detention centers are receiving substance use treatment, highlighting the need for addressing addiction early and providing recovery services in all settings. These statistics underscore the importance of diverse treatment options to meet the varying needs of individuals struggling with substance use disorders.